Leveraging Information Technology to Reduce Refeeding Syndrome Risk and Enhance Nutritional Care
Xin-Jin Lu, Dietitian, Dept. of Food & Nutrition
Refeeding syndrome (RFS) is a serious nutritional complication that occurs when patients who have been undernourished for more than 5 days resume caloric intake too rapidly. This can result in electrolyte imbalances, acute micronutrient deficiencies (such as vitamin B1 deficiency), fluid retention, and even death. Although often overlooked in clinical settings, RFS can become a life-threatening condition once it occurs.
To enhance efficiency, the Nutrition Department incorporated four key RFS risk indicators into the hospital's medical information system within the nutrition screening interface: Body Mass Index (BMI), percentage of weight loss over the past 6 months, inadequate food intake for more than 5 days, and low blood phosphorus or magnesium levels.
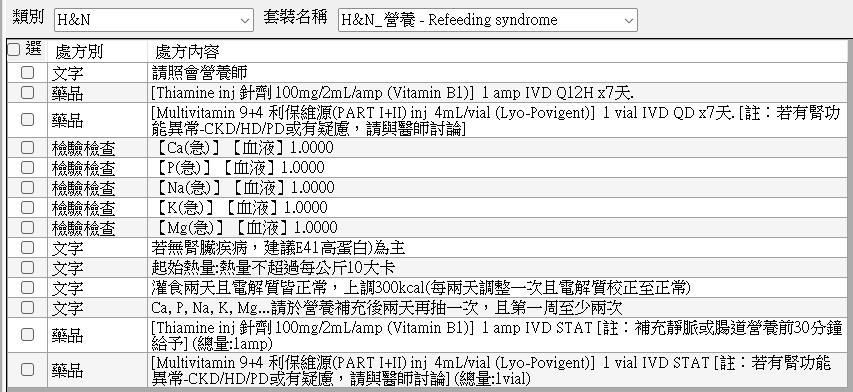
Upon patient admission and during nutritional screening, the system automatically flags those at risk for RFS, reducing screening time from 10 minutes to 1 minute. Color-coded indicators highlight at-risk patients, making alerts more visually distinct. To ensure standardized nutritional care, particularly in head and neck cancer and esophageal cancer wards where RFS incidence is higher, an RFS-specific nutritional care order set was implemented. This includes recommended vitamin supplementation dosages and duration, electrolyte monitoring parameters and frequency, and dietitian consultation guidelines, reducing the time required to complete medical orders from 5 minutes to 1 second.
By implementing computer-assisted screening and standardized order sets, the time required for clinical dietitians to retrieve information and for physicians or specialists to issue medical orders has been significantly reduced. Furthermore, the quality of care for patients at risk of RFS has improved. Specifically, the identification rate of patients at risk for RFS among clinical staff increased by 26.9%, the prescription rate of RFS-related medical orders before dietitian visits rose by 14.1%, and the incidence of electrolyte abnormalities among at-risk head and neck cancer and esophageal cancer patients decreased by 50.2%.
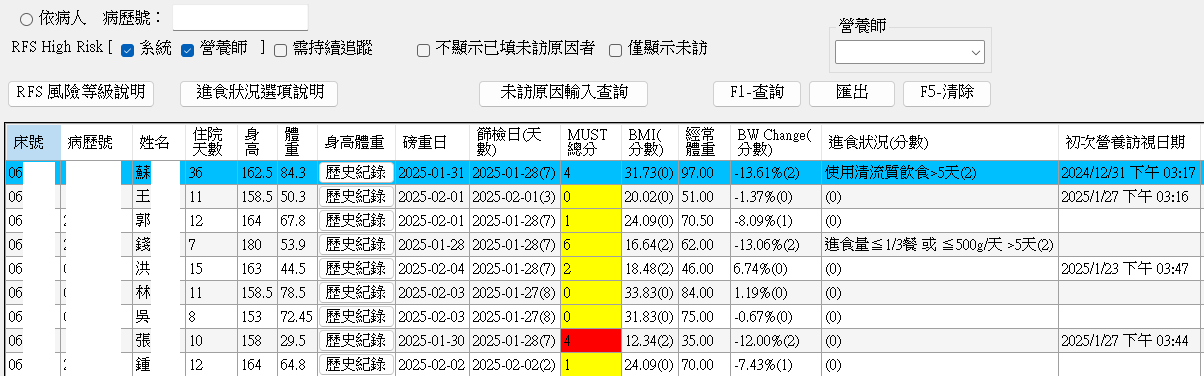
Figure 1